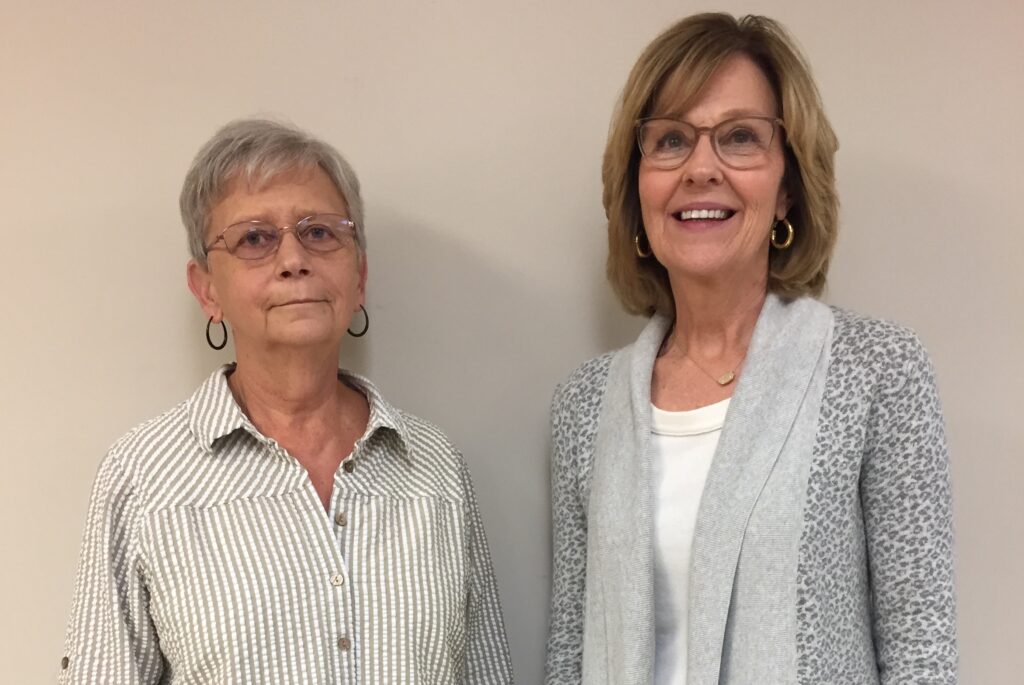
Pat Hays (L), of Leburn, Ky.; and Alice Caudill, a diabetes educator with the Kentucky River District Health Dept. in Hindman, Ky.
After first being diagnosed with prediabetes, Pat started being more intentional about walking more often, and eating more consciously—two things diabetes coaches will tell you can make a huge difference in controlling your blood sugar. And by doing this, she says, she was able to keep her prediabetes from becoming type 2 for some 10-11 years.
And even though she did eventually get a type 2 diagnosis, on learning this, Pat not only kept up her walking & eating habits, she decided to learn as much about diabetes as she could. So, she signed up for a Diabetes Self-Management Education and Support class (or DSMES, for short) at the Kentucky River District Health Department. And then she took another one. And then… she took another one.
“Even after taking one class,” she says, “there’s still so much you don’t really get, that I’ve actually done probably three. Just because every time you take it, you pick up on something else that you can learn more about.”
And as she took these classes, she made even more changes to what she eats, and how often she gets exercise. And these changes paid off: after starting DSMES classes, Pat says she’s lost some 30 lbs., weight she’s been able to keep off. And what’s more, she says, “when I started getting it under control, and [my blood sugar] was staying down more, I realized I was feeling better, and I had more energy!”
That said, managing diabetes on a day-to-day basis can still be stressful, even in normal times. Much less when something like last summer’s catastrophic East Kentucky flood happens on top of it.
In this audio story (push play above to listen, or click below for a full transcript), we hear both about Pat’s health journey in getting her blood sugar under control, as well as her personal experience during the 2022 flood— and how the flood made managing her diabetes even more difficult. We also hear in this piece from Alice Caudill, a licensed diabetes educator with the Kentucky River District Health Department (who also just so happened to be Pat’s instructor in her DSMES classes!) about Pat’s experience in learning how to better manage her blood sugar, as well as the unique difficulty of dealing with extra stress—such as last year’s catastrophic flood—when you manage diabetes.
Music in this story was performed by Glenn Jones & Laura Baird (“Across the Tappen Zee”), and by James Blackshaw (“Cloud of Unkowing” and “Cross”), all from the Free Music Archive.
My name is Alice Caudill, and I work with the diabetes program here at Kentucky River District Health Department.
[PAT]: And my name is Pat Hays. And I live about five miles up the road, at a little road called Possum Trot. Possum Trot, Kentucky! It’s actually Leburn, Ky., but I live at Possum Trot.* * *
[PAT]: Well, I’m by myself, and with rain that hard, I just couldn’t go to sleep. So I had not went to sleep. And some family members called to check on me, and had talked to me on the phone, and then we lost service, and of course I couldn’t reach anybody at that point. So, I just stayed up. The noise— the water was so loud. Because I live up on the mountain, just a little bit. But the water that came off each side of the mountain on my property was so loud— I went out with a flashlight about 2:30, I just wanted to see why it was so loud. And, I mean, water was coming right through my yard. I mean, I videoed it, it was just unreal. But of course I couldn’t go back to sleep then, for sure, because I couldn’t get up with anybody. And I didn’t… I wasn’t going to sleep knowing it was that bad.
[ALICE]: Pat went through a lot of stress during the flood. Her brother, actually, his home was washed away the night of the flood. And she can tell this better than me—but, the night of the flood, they woke up and realized the water was getting really high in their home. He and his son ran out and got the cars, moved them to higher ground. By the time he got back to his family, he couldn’t get back in the house any more. So all of his family had to go actually to the rafters. I’ll let you take up on it there– on how hard that was for him to sit there and watch them through the night.
[PAT]: Yeah, they went up into the attic. And the attic is not floored. So it was just— the wood and insulation, is all it was. And he and his son came back down and couldn’t get to the house. And the wife and grandchildren and great-grandchild couldn’t get out. So they went up, and he and the son stood across the road, not knowing what happened to them. The granddaughter was trying to yell out the attic window and let them know they were okay. But you couldn’t hear, because of the roar of the water. Nobody could hear, until 9:30 the next morning. And so nobody knew what had happened to anybody until the next morning.* * *
[PAT]: My son-in-law, who lives a mile down the road, came up the next morning to check on me. He was in, like, a side-by-side. And he checked on me, but I still couldn’t get up with my brother and them. And we couldn’t get down there because the water was up too high. And later that evening, the water went down enough that he could get down there in a truck. And he came back and told me that they had… that they had lost everything. And he told me about them being in the attic, my sister-in-law and her grandchildren and great-grandchild. And of course, that really upset me. So, probably a couple hours later, I wanted to go down and see— I just had to go see that they were okay for myself.So we went down and checked. And my grandson and the daughter and the son-in-law went into the house and got out medicine for them. Mud was so slick, you couldn’t hardly stand up, it was terrible. But they went in the house and found their medications for them. And my sister-in-law knew that they had clothes in the top shelf in closet that would be good. So they got those clothes and brought them out for them. Of course that’s when we decided they would come to my house and stay, so we went on back to my house that evening. But, it was just so stressful— I mean, that was one day I didn’t think about what I ate or what it was, I was just getting through the day. It was just unreal. Unreal.
* * *
[ALICE]: Pat does have type 2 diabetes, and she has participated in our trainings, they’re called Diabetes Self-Management Education (DSMES). And the program that we use here at our health department is called Healthy Living with Diabetes. It is an eight-hour class, that someone with type 1 or type 2 would take. The first time Pat ever took the class, it was probably back in 2015-16; she’d been diagnosed with diabetes for a couple of years. She took the class; it was four hours for two days. We had lunch together, so she learned to count her carbohydrates, and all that kind of stuff… [PAT]: Actually, I was prediabetic for about 10 or 11 years, and I controlled that by walking and diet. But I have a history of diabetes in my family—both sides of my family, mother and father—so it finally caught up with me. And that’s probably been, I’m going to guess, 12 years ago, something like that.And I really didn’t know how—I mean, I knew Alice already, and she kind of told me some stuff. And then we got started with some diabetes classes, which helped. But even after taking one class, there’s still so much you don’t really get, that I’ve actually done probably three. Just because every time you take it, you pick up on something else that you can learn more about.
So, yeah, it has definitely helped a lot. In fact, when I first started… I’m not gonna say what I weighed! But I probably weigh 30 lbs. less now than I did a couple of years ago. Because I started eating different! Oh, I ate fired potatoes, and cornbread, and things you don’t each much of when you’re diabetic. So I had to change a lot of that!
* * *
[PAT]: Instead of frying pork chops, I went to baking pork chops. And my breakfast was a big change. Before, my breakfast could’ve been a Little Debbie cake and some milk. It really might’ve been! [ALICE]: Well, something you told me at the time, and you’ve said it before, is that— she knew she wasn’t supposed to eat sugar. But she, at the time, didn’t realize what carbohydrates really were. And it wasn’t just sugar: it was flour, and it was potatoes, and— [PAT]: Yeah, it was like toast, you know! [ALICE]: And there was carbohydrate in milk. You know, there’s as much carbohydrate in a cup of milk, almost, as a piece of bread. A lot of people, that never enters their mind that there’s natural sugar in milk. So stuff like that, because the first time that you took the class, you got the book and started learning about carb counting. [PAT]: Things you don’t think about! Like she said, like the milk, and stuff like that, you don’t think about those things. [ALICE]: And one of the things that Pat learned well, is, in goal-setting, you have to be real specific. And you’re going to do that every day, and you’re going to write it down, and you’re going to ask yourself regularly, am I doing that—you have to talk about it. Because Pat made the decision to change— you know, she did want to eat healthier, but she made those specific goals: that she wasn’t going to eat fried foods anymore. And she talked about it. And she would ask for recipes. And also, at that time, we had a support group here in Knott County. And we did some recipes— she always made sure, that even though she was fixing something else for the family, she was following true to her lower-fat cooking methods for herself.* * *
[INTERVIEWER]: Is there any advice that you would give to folks who are trying to get blood sugar under control, whether they have type 2 already, whether they have prediabetes, whether they have family history— is there any advice that you would give to folks? [PAT]: Exercise regularly. Drinking water. Baking or broiling, instead of frying a lot of foods. More vegetables and fruits— watch your vegetables and fruits, rather than going to potatoes, you know, you can have a salad instead. Or green beans instead of potatoes. Something that’s healthier. [ALICE]: And you’re the queen of portion control. [PAT]: Well, I do try. [ALICE]: She is! [PAT]: I do try. Well, you have to know how much you’re going to eat of something! If you’re supposed to have—like, a normal portion of meat is, like, the palm of your hand. I wouldn’t have thought that! I mean, would’ve thought it would’ve been a piece of chicken the size of my whole hand— [ALICE]: Like about 5 or 6 ounces, when it’s really about 3. [PAT]: Yeah! You just don’t think about those things.From the time I was diagnosed, until I got it under control, I did start feeling different. I felt sluggish, just didn’t feel real good. Not a lot of energy. But then when I started getting it under control, and it was staying down more, I realized I was feeling better, and I had more energy! And… yeah. It made a difference.
* * *
[PAT]: In the beginning, you know, I was prediabetic for the 10 or 11 years. And I knew that I had family history of it. But I did keep it under control that long, before it caught up with me! But I still knew that if I was careful, I wouldn’t have to be like other members of my family that I have seen in years past, who did not take care of it. They just really didn’t try: bad eyesight, being overweight, not trying to do any better.We’d go visit somebody in the hospital, and here’s relatives coming in with cheeseburgers and french fries, and milkshakes—and I know they’re diabetic, and I’m thinking, I can’t believe you’re eating that! And one time I might’ve made a comment: I didn’t realize you could eat french fries, or something. ‘Well, I’ll take my shot.’ Well, that’s not the solution. You don’t eat what you want, and take your shot of insulin. That’s just not the way you control it! You just have to realize, I’m not going to let this control me. I’m going to get ahold of it, and do what I can with it. Because if you don’t, it will control you. So yeah, you can, you can manage it!
* * *
[INTERVIEWER]: Have you always been exercising?
[PAT]: I’ve always been an exerciser, yeah. That’s something I’ve always done. But I was more conscious of doing it every day. And there was more of a purpose to it than just doing it because I enjoyed doing it. [INTERVIEWER]: What’s sort of your routine of managing diabetes normally in terms of exercise? And did the flood affect that at all? [PAT]: Oh yeah. Yes, definitely. Because I go to silver sneakers, which is an exercise program here for seniors, I go to that usually Mondays and Thursdays. And then I try to walk the other days, I try to walk at least a half hour a day. [ALICE]: But that was at the Sportsplex. So, that was called off, because it was being used for disaster relief— [PAT]: Yeah, it changed everything. [ALICE]: FEMA went in, so you could no longer get in there to do her regular exercise. And normally you would come to church, and a lot of people walk in Hindman, because we can walk over at the Settlement School, and it’s real nice, there’s a little bridge, you can go all the way down to the library and different things… and of course, all of that was flooded. So there wasn’t walking there, for a lot of people that used that. [PAT]: Now rather than go to the Sportsplex for classes, my walking is— I live up on a hill. So, I walk down my driveway, up the highway, down the neighbors’ driveway back up. Which is harder—it’s probably better for me; it’s harder on my knees. [ALICE]: But it’s not a real safe area for you to cross the road there. [PAT]: No, it’s not! It’s not safe. It’s on a mountain. So it’s not safe.* * *
[INTERVIEWER]: Did you notice any changes in your blood sugar following the flood? [PAT]: It happened on Wednesday night, didn’t it? So on that Thursday, it was up. I think just because I was so stressed out over everything that was going on that day. The days after that, it wasn’t so bad, because I was moving around more, and I was just more conscious, and was able to find more things to eat and whatever. [ALICE]: We’ve talked about, just the stress level— of even if it wasn’t your home, that still, how you’re affected. Our literature says that there’s probably 400, or more, things you deal with every day because you have diabetes. You’re checking your blood sugar. You’re monitoring it. And if it’s high this morning, you take a fasting. And it’s high, well, why is it high? What did I eat last night? You’re totally dealing with issues every day that are stressful. But also, on top of caring for yourself and your health with diabetes, then as soon as you start adding things like what she’s been through… [INTERVIEWER]: You mentioned that your blood sugar kind of got affected in the day after [the flood], what’s it been like since? [PAT]: Some days are not as good as others. But it’s been okay. [INTERVIEWER]: Has just the stress of the situation and everything been a part of things some days? [PAT]: Yeah. That’s part of it being up, yeah.You know, in something like this, your mind tends to go to it a lot. And you have to learn to bring yourself out of that, and focus on what you have to do. That has been a chore. It’s been a challenge.
[ALICE]: Well, and, also, something that Pat did through all of this— the group that stayed at our church, we provided meals for them. Breakfast and supper. So you had be there at 5:30 to get their breakfast. And she was there sometimes that early. And she would come and help do supper— [PAT]: But if I did a lot of walking and moving around like that, then I didn’t worry about walking at home. Because I’d gotten enough exercise just during the day. And when you’re helping with the meals and stuff, you get a lot of exercise. [ALICE]: But she’s kept herself physically fit enough so that she could do that. What’s unique with Pat— she looks at the future, in saying I don’t want to sit still. I want to keep moving, I want to keep doing everything I can for others. It’s not about Pat. It’s about keeping herself healthy for other people, for service, it really is.